From the Publisher: “For more than fifty years, we have been waging, but not winning, the war on cancer. We’re better than ever at treating the disease, yet cancer still claims the lives of one in five men and one in six women in the US. The astonishing news is that up to two-thirds of all cancer cases are linked to preventable environmental causes. If we can stop cancer before it begins, why don’t we?
That was the question that motivated Kristina Marusic’s revelatory inquiry into cancer prevention. In searching for answers, she met remarkable doctors, scientists, and advocates who are upending our understanding of cancer and how to fight it. They recognize that we will never reduce cancer rates without ridding our lives of the chemicals that increasingly trigger this deadly disease.
Most never imagined this role for themselves. One scientist grew up without seeing examples of Indian-American women in the field, yet went on to make shocking discoveries about racial disparities in cancer risk. Another leader knew her calling was children’s health, but realized only later in her career that kids can be harmed by invisible pollutants at their daycares. Others uncovered surprising links between cancer and the everyday items that fill our homes and offices.
For these individuals, the fight has become personal. And it certainly is personal for Berry, a young woman whose battle with breast cancer is woven throughout these pages. Might Berry have dodged cancer had she not grown up in Oil City, Pennsylvania, in the shadow of refineries? There is no way to know for sure. But she is certain that, even with the best treatment available, her life was changed irrevocably by her diagnosis. Marusic shows that, collectively, we have the power to prevent many cases like Berry’s. The war on cancer is winnable—if we revolutionize the way we fight.”
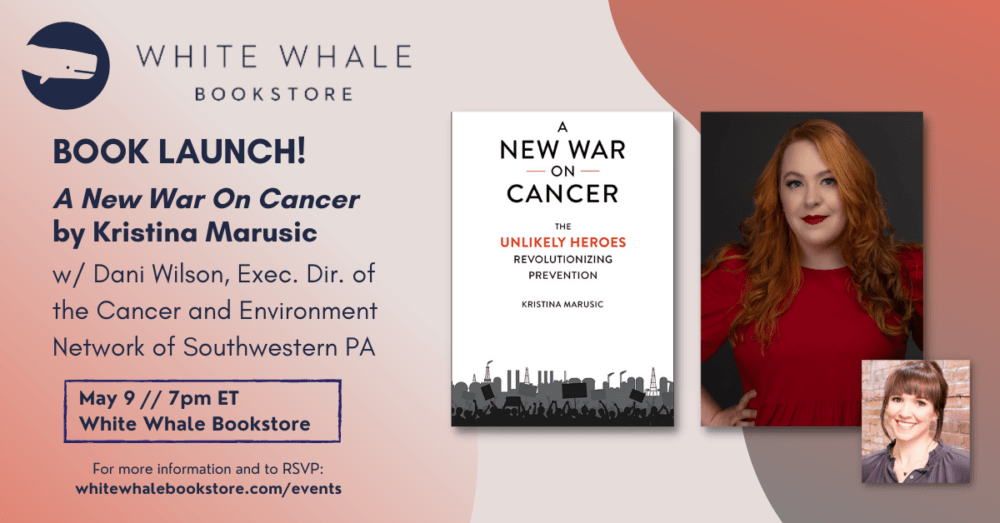
More info About the Author: Kristina Marusic is an award-winning journalist who covers environmental health and justice for Environmental Health News. She holds an MFA in nonfiction writing from the University of San Francisco, and her personal essays and reporting on topics ranging from the environment, LGBTQ+ equality, and politics to feminism, food, and travel have been published by outlets including CNN, Slate, Vice, Women’s Health, the Washington Post, MTV News, The Advocate, and Bustle , among others. She lives in Pittsburgh with her partner of ten years, Michael, and the cutest dog in the world, Mochi. You can visit her online at KristinaMarusic.com.
Author Site Don’t miss out: Kristina Marusic will be launching A New War on Cancer at White Whale on May 9th (in conversation with Dani Wilson, Executive Director of the Cancer and Environment Network of Southwestern Pennsylvania).
Book Launch “In this series of engaging profiles linked by an overarching investigation into the negative impacts of chemical pollution, readers will find themselves learning from researchers, health advocates, lawyers, and community activists about the many insidious ways cancer has been invited into our daily lives….This is a surprising and significant look at cancer research, an eye-opening book readers will feel compelled to talk about with everyone they know.” —Booklist, Starred
“In this big-hearted book, Kristina Marusic profiles the everyday champions of the most important battlefront in the ‘war on cancer’: the too-often overlooked movement to prevent environmental illness instead of just to survive it.” —Dan Fagin, author of the Pulitzer Prize-winning Toms River: A Story of Science and Salvation
“Extraordinary journalist Kristina Marusic not only makes the case for a new war on cancer, she tells deeply human stories that inspire us to think beyond the defeatist myths of consumerism and confront polluters in our own communities. Best of all, her book helps those of us already diagnosed with cancer see ourselves as determined warriors.” —Sandra Steingraber, author of Living Downstream: A Biologist’s Personal Investigation of Cancer and the Environment
“Kristina Marusic alerts us to a hidden but deadly crisis: the threat that everyday chemicals pose to our health and that of future generations. Readers can’t help but be drawn into this alarming story, vividly told through the lives of those affected.” —Shanna Swan, author of Count Down and Professor of Environmental Medicine and Public Health, Icahn School of Medicine at Mount Sinai
“For decades, the ‘war on cancer’ has neglected environmental justice and the need to rid the nation of harmful chemicals. Marusic’s dramatic account puts a human face on the struggle to right this wrong. An excellent book!” —Robert D. Bullard, Director, Bullard Center for Environmental & Climate Justice, Texas Southern University
“An urgent exposé on the need for truly comprehensive cancer prevention.” —Doris Browne, former Program Director, National Cancer Institute and 118th President, National Medical Association
Introduction
Madelina DeLuca was diagnosed with leukemia about a month before her second birthday.
“She had some bruising and we couldn’t figure out where it came from,” her mom, Kristin DeLuca, told me in 2019 when I interviewed her for a story about environmental exposures and cancer.
Madelina’s doctors ran a bevy of tests, but they didn’t reveal any answers. Then Madelina developed inexplicable stomach pain, and the dark blue and purple blooms on her skin multiplied. After several months of uncertainty, a blood test came back showing too many white blood cells. In November 2014, her doctor ordered a bone marrow biopsy. “She got a fever after the biopsy, so they kept her in the hospital as a precaution,” Kristin said. “Then it all happened really fast. Her test results came back the next day, she was diagnosed with acute myeloid leukemia, and within two days she had a port in her chest and had started chemo. It was very overwhelming.”
In 2015, while Madelina was undergoing treatment at the Children’s Hospital of Pittsburgh, a photo of her embracing another young cancer patient went viral. The image of the little girls—one dark-skinned, one pale, both wearing jammies, their nearly bald heads touching while they held each other and gazed out a hospital window at the city skyline— was shared around the world and garnered national media attention.
The other girl in the photo was five-year-old Maliya Jones. Her mother, Tazz Jones, captured the candid shot and captioned it, “This is the perfect example of love,” in a Facebook post. In media interviews at the time, Tazz expressed hope that the girls would stay friends as they got older and would have the photo to commemorate the difficulties they had both overcome.
Maliya died a year later at the age of six.
Kristin told me, “Throughout the course of Madelina’s treatment, she made a lot of friends who weren’t able to defeat it.”
Climbing Cancer Rates
The United States is more than fifty years into its “war on cancer,” but the disease is still prevalent. Half of all American men and one in three women can expect to get some type of cancer diagnosis in their lifetimes. We’re better than we’ve ever been at curing and treating the disease, but cancer still claims the lives of one in every five American men and one in every six women. Rates of some types of cancer have fallen over time, but others continue to increase.
Childhood cancer rates are particularly striking. While cancer is still relatively rare among childhood diseases, Maliya and Madelina are far from alone. One in every 285 American children receives a cancer diagnosis before the age of twenty, and cancer rates for children and teens across the US have increased steadily over the last fifty years. Rates of childhood leukemia have increased by 35%, and rates of childhood brain cancer have gone up by 33% since researchers started tracking the disease in the early 1970s. Cancer rates in children and teens across the globe have followed a similar upward trajectory.
This increase is too rapid to be the result of genetic changes alone, which would happen over centuries, not decades. Rapid increases in disease rates are sometimes explained by improvements in diagnostic capabilities. When our ability to detect a disease improves, we start finding more of it. This might account for some of the increase in childhood cancers, but it doesn’t fully explain what’s happening here. While many new tests enable us to learn more about cancer subtypes and make more accurate diagnoses, the fundamental diagnostic tools for the most common types of childhood cancers haven’t changed. So if increasing childhood cancer rates aren’t explained by genetic changes or better diagnostic tools, what’s been causing such a rapid increase for the last fifty years?
Dr. Margaret Kripke, a leading expert in the immunology of skin cancers and professor emerita of the University of Texas MD Anderson Cancer Center, served multiple terms on the US President’s Cancer Panel—a three-person panel that advises the president of the United States on high-priority issues related to cancer and oversees the development and implementation of the National Cancer Program.
In 2008, when she learned that the President’s Cancer Panel would investigate environmental causes of cancer, Kripke bristled at the idea. A single study from the 1980s indicated that pollution and chemical exposures caused just 6% of all cancers, and that statistic had been widely accepted ever since. Kripke had never questioned the findings, so she thought the group’s time would be better spent researching other aspects of cancer. But what they found during their two-year investigation left her stunned.
The panel determined that up to two-thirds of all cancer cases are linked to preventable environmental exposures (a category that includes any factor originating outside the body and our own DNA like smoking, pollution, and chemical exposures). They also learned that while around 80,000 chemicals are used in products sold to American consumers fewer than 1% have ever been tested for toxicity or safety, and existing regulations on cancer-causing chemicals in consumer products are rarely enforced. “I had a set of assumptions that most people have, that chemicals are tested before they’re put on the market, that things known to be carcinogenic are regulated, and that if regulations exist, they’re enforced,” Kripke said. “It turned out none of that is true. It was a completely eye-opening experience for me.”
In 2010, the Panel released its report on environmental exposures as causes of cancer, marking the first time the subject had been covered in the organization’s forty-year history.1 Kripke explained that while individual cases of cancer cannot be traced to harmful exposures, a substantial body of research has shown that among groups of people, less exposure equals fewer instances of cancer. Fewer cancer cases occur in communities where there is reduced exposure to cancer-causing chemicals.
“Many of the researchers who came to testify before the President’s Cancer Panel were incredibly frustrated because they had been saying this for a very long time, but nobody had been listening,” Kripke said. “That was very moving to me, and it struck me as something that was quite amiss with the field.”
The report was controversial at the time. Because of the difficulty of linking any one person’s cancer to chemicals, some of Kripke’s colleagues wanted to continue to focus exclusively on changing individual behaviors, such as diet and exercise, which she referred to as a “blamethe- victim approach to cancer prevention.”
“I heard from a young man who was just completely outraged that he’d gotten cancer despite having a perfectly healthy lifestyle,” she said. “He exercised, he never smoked, never drank, but he still developed bladder cancer. He felt like he’d been lied to. Having a healthy lifestyle is important, but it’s misleading to let people think they can control whether or not they get cancer just by having healthy lifestyles.”
Awareness about environmental exposures and cancer risk has increased since the report came out in 2010, but the fundamental problem persists. “There’s still a lot to be concerned about in the way we do business in the US, where we use a reactionary principle rather than a precautionary one—meaning we wait until there’s evidence that chemicals are causing harm before trying to regulate them,” Kripke said.
In other parts of the world, including the EU, Denmark, and Sweden, regulators evaluate potentially harmful substances before approving their use, at least in theory. In the US, Kripke said, class action lawsuits seeking compensation for people who’ve been sickened or killed by chemicals often precede regulations, or even stand in for them.
Lawsuits are often reserved for extreme cases of exposure, but in fact, we’re all regularly exposed to low doses of cancer-causing compounds in food and water, personal care products, and air pollution. We consume chemicals in the things we eat and drink, absorb them through our skin, and inhale them in the air we breathe.
Kids and teens are much more vulnerable to these constant, low-dose exposures than adults, according to Dr. Phil Landrigan, a pediatrician, public health physician, and epidemiologist who serves as director of the Global Observatory on Pollution and Health at Boston College. Kids breathe more air, eat more food, and drink more water per pound of body weight than adults, so carcinogens in their air, food, and water wind up in their bodies at higher concentrations. Because kids’ defense mechanisms aren’t yet mature, Landrigan explained, their bodies also have less ability than adults’ bodies to remove things that shouldn’t be there. And they’re still undergoing complex development processes in their brains, immune systems, and reproductive systems that make those bodily systems more vulnerable. Thousands of steps must occur in precise sequence for healthy human development; if something gets into a child’s body that disrupts those processes, even at a very low dose, it can initiate the development of disease, making kids the proverbial canaries in the coal mine.
Alarmingly, research also indicates that parents’ exposures to cancer-causing chemicals—even before a child is conceived—may increase children’s cancer risk.2
After accidents, cancer is the second leading cause of death in American children ages one to fourteen today. At the beginning of 2022, the American Cancer Society estimated that about 10,470 American children under the age of fifteen would be diagnosed with cancer the following year, and that 1,050 children would die from the disease.3
Meanwhile, rates of several types of cancer strongly linked to chemical exposures have also been on the rise in adults, as has the share of lung cancer cases showing up in people who’ve never smoked. And during the same time period, people of increasingly younger ages have started getting cancers typically seen in adults
An Ounce of Prevention
From 1988 to 1992, American scientists engaged in a fierce debate about how to prevent hundreds of babies from dying suddenly and inexplicably each year. In 1985, a groundbreaking study had revealed that sudden infant death syndrome (SIDS) was rare in Hong Kong, where cultural norms had babies sleeping almost exclusively on their backs. In 1987, the Netherlands had started a public health campaign urging parents to do the same with their infants, which had resulted in a steep decline in SIDS cases, and the UK was considering following suit. Some American researchers felt strongly that the United States should do the same. Others felt just as strongly that it should not.
The reason for their opposition? The evidence was limited, and no one in the research community had been able to determine why putting babies to sleep on their stomachs made SIDS more likely, despite a flood of funding and an influx of research aimed at figuring it out.
“Some scientists felt it was irresponsible not to wait on launching a public health campaign until we knew the exact mechanism by which stomach sleeping causes SIDS,” explained Mark Miller, coinvestigator with the Center for Integrative Research on Childhood Leukemia and the Environment at UC Berkeley and associate clinical professor and codirector of the Western States Pediatric Environmental Health Specialty Unit at the University of California San Francisco (UCSF). “Thankfully though, the ‘Back to Sleep’ camp won, and in the decades since the campaign was launched in 1994, the United States has seen a reduction in SIDS of about 50%.” More than twenty-five years later, scientists still don’t completely understand why stomach sleeping makes SIDS more likely.
Similarly, some scientists today think it’s important to wait until we know exactly how, at a cellular level, exposure to certain chemicals causes cancer before we focus resources on preventing widespread exposure to them. But we have much more evidence about environmental risk factors for childhood leukemia now than we had on SIDS when Back to Sleep was launched, and Miller, who specializes in childhood leukemia research, believes there’s a lesson to be learned there.
“Once we have identified a risk factor for cancer, do we really need to wait decades for all of the mechanisms to be fully understood before we take action?” he asked. “We know that fewer exposures to risk factors mean fewer cancer cases, and we also know we should be doing these things anyway—pesticides, air pollution, and carcinogenic chemicals in personal care products have all kinds of other risks too, especially for children, including asthma, hormone disruption, and impaired neurodevelopment.”
While many cancer experts believe the old adage holds true—that an ounce of prevention is worth a pound of cure—that’s not how we’ve tackled fighting cancer to date. It’s estimated that only 7%–9% of all global funding goes toward prevention.4 The rest of the billions of dollars funneled into the war on cancer goes toward pursuing cures and treatment.
While research on cures and treatments is critical, this imbalance is problematic. If the “war” was an actual military conflict, this would be like spending 93% of our resources to treat wounded soldiers and civilians, and spending only 7% on offensive or defensive measures that could prevent them from getting hurt in the first place.
Even when cancer prevention initiatives are funded and carried out, most focus on individual choices that can reduce risk, like not smoking, not drinking too much, eating healthy foods, and exercising. Those lifestyle choices certainly matter, but many, many people who make all the right lifestyle choices still get cancer, including increasing numbers of children, who generally aren’t smoking or drinking. Their parents’ lifestyle choices play a role, of course, but while rates of drinking and smoking during pregnancy have steadily declined, childhood cancer rates have continued to skyrocket.
Today, very little cancer funding is allocated to reducing our exposure to cancer-causing chemicals in our air, water, food, or personal care products—something that affects every single one of us, no matter how smart our lifestyle choices are.
Chemicals of Concern
New research suggests that traditional methods of screening chemicals are inadequate because they overlook the fact that humans are perpetually exposed to “acceptable” doses of many carcinogens simultaneously. They also fail to account for the chemical mixtures we’re exposed to, which can interact to create even greater cancer risk than the sum of each individual chemical exposure. And traditional screening methods miss many chemicals that raise cancer risk indirectly in a number of ways, including by disrupting our natural hormonal processes.5
These “endocrine-disrupting chemicals” are widespread, and a growing body of research links them to hormone-related cancers. Some of these cancers, including multiple myeloma and testicular cancer, have risen dramatically since the US started tracking national cancer rates in 1975, even as other types of cancer have declined in adults.6 Endocrine disruptors’ association with breast cancer risk has been particularly well documented, and researchers have found that women bear a disproportionate burden of chemical exposure. A 2021 study identified almost 300 endocrine-disrupting chemicals in everything from hair dye, lipstick, and lotion to food additives that can increase levels of breast cancer–contributing hormones.7 Endocrine-disrupting chemicals also contribute to obesity, which is cited as a primary risk factor for cancer.8
Even more troubling, when it comes to endocrine-disrupting chemicals, our exposures aren’t just our own—they can increase cancer risk over multiple generations. For example, a 2021 study linked exposure to DDT, an endocrine-disrupting pesticide, to obesity and early menstruation, both breast cancer risk factors, for at least two generations. DDT was banned in the US in 1972, but this means your mother’s exposures before the ban could increase not only her breast cancer risk, but also yours and your daughters’.9 Diethylstilbestrol (DES) is another example. The endocrine-disrupting drug was widely and ineffectively used to prevent miscarriages from 1940 to 1971, but DES was banned after scientists learned that women who took it during pregnancy had daughters with a significantly higher risk of developing rare vaginal and cervical cancers.10
We all encounter cancer-causing chemicals in our everyday lives, but research shows that some communities face higher exposures than others. Low-income communities tend to experience higher levels of air pollution than wealthier ones, for example, but research has also shown that across all income levels, Americans of color are exposed to higher levels of harmful air pollution than their white counterparts.11 These disparities, which are the result of decades of segregation and racist housing policies, are further exacerbated by other forms of racial and environmental injustice. For example, personal care products marketed to Black and Hispanic communities contain higher levels of endocrine-disrupting chemicals than products marketed to white communities. And because of the inequities in the US medical system, people of color often have worse cancer outcomes—for instance, Black women are 41% more likely to die from breast cancer than white women.
A New Story
I first learned Madelina’s story and started researching environmental causes of cancer while working as the Pittsburgh correspondent for Environmental Health News, a national nonprofit news outlet focused on how changes in the environment affect human health. I’d taken the job because the organization’s mission resonated with me on a personal level.
My own family has had its share of health problems. My dad, who grew up in Pittsburgh, survived a benign but difficult-to-remove brain tumor a decade ago. My younger sister, who has lived in Pittsburgh for nearly two decades, is in remission from thyroid cancer after being diagnosed at the age of twenty-five. My husband, who grew up in the region, has a rare autoimmune disorder, and his family has also struggled with various diseases, including cancer. I couldn’t help but wonder whether all of their illnesses might have a common thread— especially given the area’s industrial past and ongoing problems with air pollution.
Through the course of my reporting, I learned that while it’s not yet possible to determine the exact causes of one person’s cancer, scientists have identified eight “cancer hallmarks”—or specific changes to cells— that need to happen for cancer to develop.12 Each of these hallmarks happens through complex interactions between genetic and external factors, including exposure to carcinogenic chemicals.
I also learned that cancer isn’t typically caused by a single event or environmental exposure, but a unique set of conditions and events that produces cancer in an individual person. One emerging theory is that cancer risk is like a pie chart with a different cancer cause in each slice— things like inherited genetics and gene mutations, your parents’ and grandparents’ chemical exposures, and your various potential exposures to things like cigarette smoke, air pollution, or cancer-causing chemicals in food or drinking water. Everyone’s pie looks a little different, but if just one piece goes missing, cancer won’t develop in that person.
This made me wonder—are there slices of my loved ones’ pie charts that wouldn’t be there if their childhood zip codes had been different? If they hadn’t lived in the shadow of steel mills and coal-fired power plants, would they have remained healthy? I don’t smoke, and I try to eat healthily and exercise, but what about factors beyond my control? What slices had started filling in since I’d moved to Pittsburgh, or while I was living in Taiwan, or New York, or San Francisco?
As I continued learning about all the ways Americans are exposed to cancer-causing chemicals in our air, food, water, and personal care products, I found myself frequently overwhelmed by the enormity of the problem. Yes, I could take some steps to reduce my exposure—shopping organic when I could, paying attention to the ingredients in my shampoo and lotion and makeup, using a water filter—but I couldn’t wall myself off from most chemicals. It was a realization that prompted feelings of powerlessness.
But then I discovered a national network of brilliant people working diligently to solve this problem. They are researchers, scientists, physicians, policy wonks, and concerned parents. Their numbers are still small, but their efforts are ambitious, broad in scale, and focused on systemic change—because we as individuals cannot simply shop our way out of a problem this pervasive.
Many of these efforts are being undertaken by a national coalition dubbed the Cancer Free Economy Network, which has the lofty goal of drastically reducing cancer rates by shifting the economy away from the widespread use of carcinogenic chemicals and toward safe alternatives. Since its founding in 2014, more than sixty groups and individuals have joined the Cancer Free Economy Network, including a host of health advocacy, academic, labor, environmental, and business groups, along with prominent physicians, entrepreneurs, and policy experts.
One of the network’s prime directives is changing the way Americans think and talk about cancer. Progress on prevention has been slowed by pervasive cultural myths about cancer, like the notion that cancer risk is only about genetics or luck (“My grandma smoked three packs a day for forty years and never got sick.”), or the idea that “everything causes cancer” so it’s pointless to worry about trying to minimize exposure. In truth, it’s well proven that reducing a community’s exposure to carcinogens consistently reduces its number of cancer cases over time, and that focusing on prevention in ways that go beyond personal lifestyle choices can save many lives. There are also researchers, doctors, and advocates working on this issue separately from the Cancer Free Economy Network. Collectively, they form a national movement aimed at waging a new war on cancer—one that prioritizes offense and defense in addition to improving treatments for those wounded by the disease, with an emphasis on racial and environmental justice.
In the course of my reporting, I’ve learned the stories of both people battling cancer and people leading this movement, some of which I’m sharing in these pages. These stories aren’t just about treatments or research, they’re also personal histories: the familial threads and formative memories that created the reserves from which these unlikely heroes draw their resilience and ambition. Getting to know these people has given me strength to go beyond worrying about my personal consumption habits to join others pushing for change that will make the world healthier for all of us. I hope this book will do the same for you.
From A New War on Cancer: The Unlikely Heroes Revolutionizing Prevention by Kristina Marusic. Copyright ©2023 by Kristina Marusic. Reproduced by permission of Island Press, Washington, D.C.
Footnotes
- LaSalle D. Leffall and Margaret L. Kripke, Reducing Environmental Cancer Risk: What We Can Do Now (Washington, DC: The President’s Cancer Panel, 2008), https://deainfo.nci.nih.gov/advisory/pcp/annualReports/pcp08-09rpt/PCP_Report_08-09_508.pdf.
- Todd P. Whitehead et al., “Childhood Leukemia and Primary Prevention,” Current Problems in Pediatric and Adolescent Health Care 46, no. 10(2016.): 317–52, https://doi.org/10.1016/j.cppeds.2016.08.004.
- “Key Statistics for Childhood Cancers,” American Cancer Society, accessed January 12, 2021, https://www.cancer.org/cancer/cancer-in-children/key-statistics.html.
- Madeline Drexler, “The Cancer Miracle Isn’t a Cure: It’s Prevention,”Harvard Public Health Magazine, October 8, 2019, https://www.hsph.harvard.edu/magazine/magazine_article/the-cancer-miracle-isnt-a-cure-its-prevention/.
- William H. Goodson et al., “Testing the Low Dose Mixtures Hypothesis from the Halifax Project,” Reviews on Environmental Health 35, no. 4 (August 24, 2020): 333–57, https://doi.org/10.1515/reveh-2020-0033.
- Molly Jacobs, Polly Hoppin, and Maggie Kuzemchak, Environmental Chemicals and Cancer, a Science Companion Document (Pittsburgh, PA:Cancer and Environment Network of Southwestern Pennsylvania, 2021), 194 notes https://censwpa.org/wp-content/uploads/2021/07/Science-Companion-Document.pdf.
- Bethsaida Cardona and Ruthann A. Rudel, “Application of an In Vitro Assay to Identify Chemicals That Increase Estradiol and Progesterone Synthesis and Are Potential Breast Cancer Risk Factors,” Environmental Health Perspectives 129, no. 7 (July 21, 2021): 077003, https://doi.org/10.1289/ehp8608.
- Tim Lobstein and Kelly D. Brownell, “Endocrine‐Disrupting Chemicals and Obesity Risk: A Review of Recommendations for Obesity Prevention Policies,” Obesity Reviews 22, no. 11 (August 18, 2021), https://doi.org/10.1111/obr.13332.
- Piera M. Cirillo et al., “Grandmaternal Perinatal Serum DDT in Relation to Granddaughter Early Menarche and Adult Obesity: Three Generations in the Child Health and Development Studies Cohort,” Cancer Epidemiology Biomarkers & Prevention 39, no. 8 (August 1, 2021), https://doi.org/10.1158/1055-9965.epi-20-1456.
- “Impact of EDCs on Hormone-Sensitive Cancer,” Endocrine Society, accessed January 14, 2021, https://www.endocrine.org/topics/edc/what-edcs-are/common-edcs/cancer.
- Christopher Tessum et al., “PM2.5 Polluters Disproportionately and Systemically Affect People of Color in the United States,” Science Advances 7, no. 18 (April 28, 2021): eabf4491, https://doi.org/10.1126/sciadv.abf4491.
- Douglas Hanahan and Robert A. Weinberg, “Hallmarks of Cancer: The Next Generation,” Cell 144, no. 5 (March 4, 2011): 646–74, https://doi.org/10.1016/j.cell.2011.02.013.